Orthohantavirus
| Orthohantavirus | |
|---|---|
| |
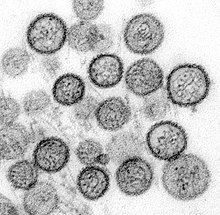
| Transmission electron micrograph of Sin Nombre virus | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Ellioviricetes |
| Order: | Bunyavirales |
| Family: | Hantaviridae |
| Subfamily: | Mammantavirinae |
| Genus: | Orthohantavirus |
| Species | |
| Synonyms[1] | |
| |
Orthohantavirus is a genus of viruses that includes all hantaviruses (family Hantaviridae) that cause disease in humans. Orthohantaviruses, hereafter referred to as hantaviruses, are naturally found primarily in rodents. In general, each hantavirus is carried by one rodent species and each rodent that carries a hantavirus carries one hantavirus species. Hantaviruses in their natural reservoirs usually cause an asymptomatic, persistent infection. In humans, however, hantaviruses cause two diseases: hemorrhagic fever with renal syndrome (HFRS) and hantavirus pulmonary syndrome (HPS). HFRS is mainly caused by hantaviruses in Africa, Asia, and Europe, called Old World hantaviruses, and HPS is usually caused by hantaviruses in the Americas, called New World hantaviruses.
Hantaviruses are transmitted mainly through aerosols and droplets that contain rodent excretions, as well as through contaminated food, bites, and scratches. Environmental factors such as rainfall, temperature, and humidity influence transmission. Human-to-human transmission does not occur. HFRS is marked by kidney disease with kidney swelling, excess protein in urine, and blood in urine. The case fatality rate of HFRS varies from less than 1% to 15% depending on the virus. A mild form of HFRS often called nephropathia epidemica is often caused by Puumala virus and Dobrava-Belgrade virus. For HPS, initial symptoms are flu-like, with fever, headache, and muscle pain, followed by sudden respiratory failure. HPS has a much higher case fatality rate than HFRS, at 30–60%. For both HFRS and HPS, illness is the result of increased vascular permeability, decreased platelet count, and overreaction of the immune system.
Individual hantavirus particles (virions) are usually spherical and vary at 70–350 nanometers in diameter. They consist of the viral RNA, which is segmented into three parts and encased in helical nucleocapsids to form three ribonucleoprotein (RNP) complexes. Attached to each RNP is a viral RNA-dependent RNA polymerase (RdRp). RNPs are surrounded by a lipid envelope that has spike proteins emanating from its surface. Each part of the viral genome is single-stranded negative-sense RNA. The segments encode one protein each: RdRp, which performs transcription and replication of the genome, a glycoprotein precursor, which is formed into surface spikes on the envelope, and the N protein, which binds to and protects viral RNA. Some hantaviruses encode on the same segment as the N protein a non-structural protein that inhibits host interferon production.
Hantavirus replication begins by attaching to the surface of cells, usually vascular endothelial cells and macrophages. They then enter the cell and form vesicles to be transferred to endosomes and lysosomes. The viral envelope fuses with the membranes of endosomes and lysosomes, which empties the viral RNPs into the host cell's cytoplasm. RdRp then transcribes the viral genome to produce messenger RNA (mRNA) for translation by host ribosomes to produce viral proteins. RdRp also produces copies of the viral genome for progeny viruses. Old World hantavirus virions are constructed in the Golgi apparatus and obtain their envelope from the Golgi apparatus, before being transported to the cell membrane to leave the cell via exocytosis. New World hantavirus virions are constructed near the cell membrane, obtain their envelope from the cell membrane, and leave the cell by budding from its surface.
Hantaviruses were first discovered following the Korean War. During the war, HFRS was a common ailment in soldiers stationed near the Hantan river. In 1978 in South Korea, the first hantavirus was isolated, Hantaan virus, and was shown to be responsible for the outbreak during the war. Within a few years, other hantaviruses that cause HFRS were discovered throughout Eurasia. In 1982, the World Health Organization gave HFRS its name, and in 1987, hantaviruses were classified for the first time, and they collectively bear the name of Hantaan virus and the Hantan river. In 1993, an outbreak of HPS occurred in the Four Corners region in the United States, which led to the discovery of pathogenic New World hantaviruses and the second disease caused by hantaviruses. Since then, hantaviruses have been found not just in rodents but also shrews and bats.
Disease
[edit]Hantaviruses are sorted into Old World hantaviruses (OWHVs), which typically cause hemorrhagic fever with renal syndrome (HFRS) in Africa, Asia, and Europe, and New World hantaviruses (NWHVs) which are associated with hantavirus pulmonary syndrome (HPS) in the Americas. The case fatality rate of HFRS ranges from less than 1% to 15%, while for HPS it is 30–60%.[2][3][4][5] The severity of symptoms of HFRS varies depending on the virus: Hantaan virus causes severe HFRS, Seoul virus moderate HFRS, Puumala virus mild HFRS,[6] and Dobrava-Belgrade virus infection varies from mild to severe depending on genotype.[7] The mild form of HFRS caused by Puumala virus and Dobrava-Belgrade virus is often called nephropathia epidemica (NE).[8][9] Repeated infections of hantaviruses have not been observed, so recovering from infection likely grants life-long immunity.[10][11]
HFRS is characterized by five phrase: febrile, hypotensive, low urine production (oliguria), high urine production (polyuria), and recovery. Symptoms usually occur 12–16 days after exposure to the virus.[12] Acute kidney disease occurs with kidney swelling, excess protein in urine (proteinuria), and blood in urine (hematuria). Other symptoms include headache, lower back pain, nausea, vomiting, diarrhea, bloody stool, the appearance of spots on the skin (petechiae), and hemorrhaging in the respiratory treact.[2][13] Renal failure leads oliguria, and restoration of kidney health comes with polyuria.[2][6] Recovery typically takes a few months.[14] In more mild cases, the different phases of HFRS may be hard to distinguish,[15] or some phases may be absent, while in more severe cases, the phases may overlap.[6]
HPS is mainly caused by two viruses: Andes virus and Sin Nombre virus. The disease has three phases: prodromal (early), cardiopulmonary, and recovery. Symptoms occur about 1–8 weeks after exposure to the virus. Early symptoms include fever, headache, muscle pain, shortness of breath (dyspnea), and low platelet count (thrombocytopenia). During the cardiopulmonary phase, there is elevated heart rate (tachycardia), irregular heartbeats (arrhythmias), and cardiogenic shock. Pulmonary capillary leakage can lead to acute respiratory distress syndrome, buildup of fluids in the lungs (pulmonary edema), hypotension, and buildup of fluid in the chest cavity (pleural effusion). These symptoms can cause sudden death.[2][5][16] After the cardiopulmonary phase is resolved, polyuria occurs while recovery takes months.[16] While HFRS is associated with renal disease and HPS with cardiopulmonary disease, HFRS may sometimes include cardiopulmonary symptoms associated with HPS and HPS may sometimes include renal symptoms associated with HFRS.[16][17]
Transmission
[edit]Hantaviruses that cause illness in humans are mainly transmitted by rodents. In rodents, hantaviruses usually cause an asymptomatic, persistent infection. Infected animals can spread the virus to uninfected animals through aerosols or droplets from their feces, urine, saliva,[6] and blood,[18] through consumption of contaminated food, from virus particles shed from skin or fur,[19] via grooming,[5] or through biting and scratching. Hantaviruses can also spread through the fecal-oral route and across the placenta during pregnancy from mother to child. They can survive for 10 days at room temperature,[2] 15 days in a temperate environment,[8] and more than 18 days at 4 degrees Celsius (39.2 degrees Fahrenheit), which aids in the transmission of the virus.[2] Environmental conditions favorable to the reproduction and spread of rodents are known to increase disease transmission.[3] Living in a rural environment, in unhygienic settings, and interacting with environments shared with hosts are the biggest risk factors for infection, especially people who are hikers[6] farmers and forestry workers,[8] as well as those in mining, the military,[19][20] and zoology.[16]
Rodents can transmit hantaviruses to humans through aerosols or droplets from the excretions and through consumption of contaminated food. Rodent bites and scratches are also an important means of transmission to humans. The prevalence of hantavirus among rodent breeders and rodent pet owners is up to 80%. In one outbreak in North America in 2017, Seoul virus infected 31 people through contact with pet rats. Andes virus has often been claimed by researchers to be the only hantavirus known to be spread from person to person, usually after coming into close contact with an infected person. It can also reportedly spread through human saliva, airborne droplets from coughing and sneezing, and to newborns through breast milk and the placenta.[2] A 2021 systematic review, however, found human-to-human transmission of the Andes virus to not be strongly supported by evidence but nonetheless possible in limited circumstances, especially between close household contacts such as sexual partners.[3][21] There is also suspicion that Puumala virus can spread from person to person through blood and platelet transfusions.[22]
Hantaviruses that cause HFRS can be transmitted through the bites of mites and ticks.[23] Research has also shown that pigs can be infected with Hantaan virus without severe symptoms and sows can transmit the virus to offspring through the placenta. Pig-to-human transmission may also be possible, as one swine breeder was infected with hantavirus with no contact with rodents or mites. Hantaan virus and Puumala virus have been detected in cattle, deer, and rabbits, and antibodies to Seoul virus have been detected in cats and dogs, but the role of these hosts for hantaviruses is unknown.[2] Infection in these other animals can potentially facilitate the evolution of hantaviruses by genome reassortment.[16] In addition to rodents, some hantaviruses are found in small insectivorous mammals, such as shrews and bats.[9][16] Hantavirus antigen has also been detected in a variety of bird species, indicative of infection.[23]
Man-made built environments are important in hantavirus transmission. Deforestation and excess agriculture may destroy rodents' natural habitat.[16] The expansion of agricultural land is associated with a decline in predator populations, which enables hantavirus host species to use farm monocultures as nesting and foraging sites. Agricultural sites built in close proximity to rodents' natural habitats can facilitate the proliferation of rodents as they may be attracted to animal feed.[18][24] Sewers and stormwater drainage systems may be inhabited by rodents, especially in areas with poor solid waste management. Maritime trade and travel have also been implicated in the spread of hantaviruses.[18] Research results are inconsistent on whether urban living increases or decreases hantavirus incidence.[24] Seroprevalence, which shows past infection to hantavirus, is consistently higher in occupations and areas that have greater exposure to rodents.[21] Poor living conditions on battlefields, in military camps, and in refugee camps make soldiers and refugees at great risk of exposure as well.[20]
Environment
[edit]
Rodent species that carry hantaviruses inhabit a diverse range of habitats, including desert-like biomes, equatorial and tropical forests, swamps, savannas, fields, and salt marshes.[18] The seroprevalence of hantaviruses in their host species has been observed to range from 5.9% to 38% in the Americas, and 3% to about 19% worldwide, depending on testing method and location.[19][25] In some places, such as South Korea, routine trapping of wild rodents is performed to surveil hantavirus circulation.[4] High humidity can benefit rodent populations in warm climates, where it may positively impact plant growth and thus food availability.[18] Increased forest coverage is associated with increased hantavirus incidence, particularly in Europe.[24]
Climate change and environmental degradation increase contact areas between rodent hosts and humans, which increases potential exposure to hantaviruses. An example of this was the 1993 Four Corners outbreak in the United States, which was immediately preceded by elevated rainfall from the 1992-1993 El Niño warming period. This caused a substantial growth in the food supply for rodents, which led to rapid growth in their population and facilitated greater spread of the hantavirus that caused that outbreak.[18][19][26]
Rainfall is consistently associated with hantavirus incidence in various patterns. Heavy rainfall is a risk factor for outbreaks in the following months,[10] but may negatively affect incidence by flooding rodent burrows and nests.[26] In places that have wet and dry seasons, infections are more common in the wet season than in the dry season.[18] Low rainfall and drought are associated with decreased incidence since such conditions result in a smaller rodent population,[26] but displacement of rodent populations via drought or flood can lead to an increase in rodent-human interactions and infections.[18] In Europe, however, no association between rainfall and disease incidence has been found.[26]
Temperature has varying effects on hantavirus transmission. Higher temperatures create unfavorable environments for virus survival and decreases activity levels of Neotropic rodents, but it can cause rodents to seek shelter from heat in human settings and is beneficial for aerosol production.[16][18] Lower temperature can prolong virus survival outside a host.[18] Higher average winter temperature is associated with reduced survival of bank voles, the natural reservoir of Puumala virus, but increased survival of striped field mice in China, the natural reservoirs of Hantaan virus.[26] Extreme temperatures, whether hot or cold, are associated with lower disease incidence.[10]
Genome and structure
[edit]The genome of hantaviruses is segmented into three parts: the large (L), medium (M), and small (S) segments. Each part is a single-stranded negative-sense RNA strand and consists of of 10,000–15,000 nucleotides in total.[5] The segments form into circles via non-covalent bonding of the ends of the genome.[27] The L segment is about 6.6 kilobases (kb) in length[19] and encodes a viral RNA-dependent RNA polymerase (RdRp), which mediates transcription and replication of viral RNA. The M segment, about 3.7 kb in length,[19] encodes a glycoprotein precursor that is co-translated and cleaved into Gn and Gc. Gn and Gc bind to cell receptors, regulate immune responses, and induce protective antibodies. The S segment is around 2.1 kb in length[19] and encodes the nucleocapsid protein N, which binds to and protects viral RNA. An open reading frame in the N gene on the S segment[28] of some orthohantaviruses also encodes the non-structural protein NS that inhibits interferon production in host cells. The untranslated regions at the ends of the genome are highly conserved and participate in the replication and transcription of the genome.[2][5][6]
Individual hantavirus particles (virions) are usually spherical, but may be oval, pleomorphic,[29] or tubular.[5] The diameter of the virion is 70–350 nanometers (nm).[19] The outer part of the virion is a lipid envelope that is about 5 nm thick. Embedded in the envelope are the surface spike glycoproteins Gn and Gc,[2] which are arranged in a lattice pattern.[19] Each surface spike is composed of a tetramer of Gn and Gc (four units each) that has four-fold rotational symmetry, and extends about 10 nm out from the envelope.[19] Gn forms the stalk of the spike and Gc the head.[5] Inside the envelope are helical nucleocapsids made of many copies of the nucleocapsid protein N, which are attached to the virus's genome to form ribonucleoprotein (RNP) complexes. Each RNP complex has a copy of RdRp attached to it.[2] Hantaviruses do not encode matrix proteins to assist with structuring the virion, so how surface proteins organize into a sphere with a symmetrical lattice is not yet known.[30]
Life cycle
[edit]
Vascular endothelial cells and macrophages are the primary cells infected by hantaviruses.[9] Podocytes, tubular cells, dendritic cells, and lymphocytes can also be infected.[2][16] Attachment and entry into the host cell is mediated by the binding of the viral glycoprotein spikes to host cell receptors, particularly β3 integrins. Decay acceleration factors, complement receptors, and, for New World hantaviruses, protocadherin-1 have also been proposed to be involved in attachment.[16][30] After attachment, hantaviruses rely on several ways to enter a cell, including micropinocytosis, clathrin-independent receptor-mediated endocytosis and cholesterol- or caveolae-dependent endocytosis.[2][5][16] Old World hantaviruses use clathrin-dependent endocytosis while New World hantaviruses use clathrin-independent endocytosis.[16][22][31]
After entering a cell, virions form vesicles that are transported to early endosomes, then late endosomes and lysosomal compartments. A decrease in pH then causes the viral envelope to fuse with the endosome or lysosome.[19][22][31] This fusion releases viral ribonucleoprotein complexes into the cell cytoplasm, which initiates transcription and replication by RdRp.[2][16][19] RdRp transcribes viral -ssRNA into complementary positive-sense strands, then snatches 5′ ("five prime") ends of host messenger RNA (mRNA) to prepare mRNA for translation by host ribosomes to produce viral proteins.[5][19] Complementary RNA strands are also used to produce copies of the genome, which are encapsulated by N proteins to form RNPs.[2][16][19]
During virion assembly, the glycoprotein precursor is cleaved in the endoplasmic reticulum into the Gn and Gc glycoproteins by host cell signal peptidases.[2][5] Gn and Gc are modified by N-glycan chains, which stabilize the spike structure and assist in assembly in the Golgi apparatus for Old World hantaviruses[2] or at the cell membrane for New World hantaviruses.[16] Old World hantaviruses obtain their viral envelope from the Golgi apparatus and are then transported to the cell membrane in vesicles to leave the cell via exocytosis. On the other hand, New World hantavirus RNPs are transported to the cell membrane, where they bud from the surface of the cell to obtain their envelope and leave the cell.[16][19][22]
Evolution
[edit]The most common form of evolution for hantaviruses is mutations through single nucleotide substitutions, insertions, and deletions.[2] Hantaviruses are usually restricted to individual natural reservoir species and evolve alongside their hosts,[2] but this one-species-one-hantavirus relationship is not true for all hantaviruses. The exact evolutionary history of hantaviruses is likely obscured by many instances of genome reassortment, host spillover, and host-switching.[32] Within species, geography has affected the evolution of hantaviruses. For example, Hantaan virus and Seoul virus have both formed multiple lineages corresponding to their geographic distribution.[2]
Because hantaviruses have segmented genomes, they are capable of genetic recombination and reassortment in which segments from different viruses can combine to form new viruses. This occurs often in nature and facilitates the adaptation of hantaviruses to multiple hosts and ecosystems. Recombination in OWHVs of the S and M segments is usually observed amongst viruses within species, but can occur between species. Reassortment in NWHVs of the S and M segments has been observed in rodents. Among Puumala viruses isolated from rodents in 2005-2009, 19.1% of them were identified as reassortments.[2][33] Diploid progeny are also possible, in which virions may possess two of the same segment from two parent viruses.[34]
Classification
[edit]Orthohantavirus belongs to the family Hantaviridae, which contains all hantaviruses. The genus has 35 species, listed hereafter with the exemplar virus of the species. In general, species bear the name of the exemplar virus with the suffix -ense.[27][35]
- Orthohantavirus andesense, Andes virus
- Orthohantavirus artybashense, Artybash virus
- Orthohantavirus asamaense, Asama virus
- Orthohantavirus asikkalaense, Asikkala virus
- Orthohantavirus bayoui, Bayou virus
- Orthohantavirus boweense, Bowé virus
- Orthohantavirus brugesense, Bruges virus
- Orthohantavirus caobangense, Cao Bằng virus
- Orthohantavirus carrizalense, Carrizal virus
- Orthohantavirus chocloense, Choclo virus
- Orthohantavirus dabieshanense, Dàbiéshān virus
- Orthohantavirus delgaditoense, Caño Delgadito virus
- Orthohantavirus dobravaense, Dobrava-Belgrade virus[note 1]
- Orthohantavirus fugongense, Fúgòng virus
- Orthohantavirus hantanense, Hantaan virus
- Orthohantavirus jejuense, Jeju virus
- Orthohantavirus kenkemeense, Kenkeme virus
- Orthohantavirus khabarovskense, Khabarovsk virus
- Orthohantavirus lankaense, Lanka virus
- Orthohantavirus luxiense, Lúxī virus
- Orthohantavirus mamorense, Rio Mamoré virus
- Orthohantavirus maporalense, Maporal virus
- Orthohantavirus montanoense, Montaño virus
- Orthohantavirus nigrorivense, Black Creek Canal virus
- Orthohantavirus prospectense, Prospect Hill virus
- Orthohantavirus puumalaense, Puumala virus
- Orthohantavirus rockportense, Rockport virus
- Orthohantavirus sangassouense, Sangassou virus
- Orthohantavirus seoulense, Seoul virus
- Orthohantavirus sinnombreense, Sin Nombre virus
- Orthohantavirus tatenalense, Tatenale virus
- Orthohantavirus thailandense, which contains Anjozorobe virus and Thailand virus[note 2]
- Orthohantavirus tigrayense, Tigray virus
- Orthohantavirus tulaense, Tula virus
- Orthohantavirus wufangense, Wùfeng Chodsigoa smithii orthohantavirus 1
Many other hantaviruses are unclassified, though some may be isolates of other viruses:[27][36]
- Academ virus
- Adler virus
- Alto Paraguay virus
- Amga virus/Seewis virus[37]
- Anajatuba virus
- Ash River virus
- Asturias virus
- Azagny virus
- Belgrade virus
- Biya river virus
- Bloodland Lake virus
- Blue River virus
- Boginia virus
- Calabazo virus
- Camp Ripley virus
- Castelo dos Sonhos virus
- CGRn9415 virus
- Dode virus
- El Moro Canyon virus
- Fox Creek virus
- Fusong virus
- Gōu virus
- hantavirus sp. strain Tamarin/BRA/SM22/2014
- HoJo virus
- Iamonia virus
- Isla Vista virus
- Jemez Springs virus
- Jerboa hantavirus
- Jurong virus
- Kielder hantavirus
- Laguna Negra virus
- Landiras virus
- Leakey virus
- Lechiguanas virus
- Liánghé virus
- Lohja virus
- Malacky virus
- Muleshoe virus
- Necocli virus
- Orán virus
- Oxbow virus
- Ozark virus
- Playa de Oro virus
- Powell Butte virus
- Prairie vole virus
- Qiān Hú Shān virus/Qiāndǎo Lake virus
- Rio Mearim virus
- Río Segundo virus
- Sapporo rat virus
- Sarufutsu virus
- Serang virus
- Shěnyáng virus
- Taimyr virus
- Tanganya virus
- Tualatin River virus
- Uurainen virus
- Vladivostok virus
- Yakeshi virus
- Yuánjiāng virus
History
[edit]Hantavirus hemorrhagic disease was likely first described in the Yellow Emperor's Internal Canon in Imperial China during the Warring States Period of 475–221 BCE.[32] Hantaviruses have been suggested as a cause of "trench nephritis" in soldiers during the US Civil War and in British soldiers in Flanders, Belgium[32] during the First World War. The disease was also mentioned in East Asia, where it was probably endemic, and was first described scientifically in Vladivostok in 1913–1914. During the Second World War in 1942, an outbreak of disease with symptoms characteristic of hantavirus infection occurred in Salla, Eastern Lapland, Finland among German and Finnish soldiers. This outbreak was later reported in 1980 to be caused by a virus transmitted by bank voles and was named Puumala virus.[20] Also during the war, around 10,000 Japanese soldiers stationed in Manchuria developed HFRS.[6]
Around 3,200[20] cases of HFRS occurred among United Nations soldiers stationed near the Hantan river[30] during the Korean War, where it was first identified in 1951[2] and named "Korean hemorrhagic fever" and "epidemic hemorrhagic fever".[32] After the war, in 1976 in South Korea, Ho-Wang Lee (Korean: 이호황)[14] tested striped field mice and showed that antigens from their lungs were reactive to antibodies in sera from war survivors.[32] In 1978, the virus was isolated for the first time and named Hantaan virus after the river.[13] Retrospective analysis showed that Hantaan virus was responsible for the war outbreak.[20] Other hantaviruses that caused by HFRS were then discovered throughout Eurasia. The disease had a variety of names, so in 1982, the World Health Organization officially named it "hemorrhagic fever with renal syndrome".[6][32] In 1985, this group of viruses were named "hantaviruses" after Hantaan virus,[29] and in 1987, the genus Hantavirus was established to accommodate them in the then-family Bunyaviridae.[1]
In 1993, an outbreak of highly lethal acute respiratory distress syndrome occurred in the Four Corners region of the United States. This outbreak was determined to be caused by a hantavirus, now named Sin Nombre virus, and represented the first confirmed instance of pathogenic hantaviruses in the Americas as well as the discovery of a new type of disease caused by hantaviruses. The new disease was named "hantavirus pulmonary syndrome". During subsequent years, numerous other hantaviruses were discovered in the Americas,[5][32] including Andes virus, which has been claimed to be transmissible from person to person.[3] HFRS, however, remains much more common than HPS—more than 100,000 cases of HFRS occur each year,[24] compared to only a few hundred cases of HPS annually.[38]
Over time, hundreds of bunyaviruses were discovered but could not be accommodated within the genera of the Bunyaviridae family. To address this, in 2017 bunyaviruses were elevated to the rank of order, Bunyavirales, and hantaviruses, along with the other bunyavirus genera, were elevated to the rank of family. Hantaviruses, also called hantavirids, now also refer to members of the family Hantaviridae. The prior genus of Hantavirus was renamed Orthohantavirus to distinguish them from members of the family, and the genus's members are often called orthohantaviruses. In 2019, additional genera, subfamilies, and families were created to classify non-rodent hantaviruses,[32] and in 2023 binomial nomenclature was adopted for hantaviruses.[2]
Notes
[edit]- ^ The exemplar virus of Orthohantavirus dobravaense is Dobrava virus, a genotype of Dobrava-Belgrade. In scientific papers, "Dobrava-Belgrade virus" is essentially used as a synonym for Orthohantavirus dobravaense.
- ^ Orthohantavirus thailandense bears the name of Thailand virus but its exemplar virus is Anjozorobe virus.
References
[edit]- ^ a b "History of the taxon: Genus: Orthohantavirus (2023 Release, MSL #39)". ictv.global. International Committee on Taxonomy of Viruses. Retrieved 10 January 2025.
- ^ a b c d e f g h i j k l m n o p q r s t u v w Chen R, Gong H, Wang X, Sun M, Ji Y, Tan S, Chen J, Shao J, Liao M (8 August 2023). "Zoonotic Hantaviridae with Global Public Health Significance". Viruses. 15 (8): 1705. doi:10.3390/v15081705. PMC 10459939. PMID 37632047.
- ^ a b c d Toledo J, Haby MM, Reveiz L, Sosa Leon L, Angerami R, Aldighieri S (17 October 2022). "Evidence for Human-to-Human Transmission of Hantavirus: A Systematic Review". J Infect Dis. 226 (8): 1362–1371. doi:10.1093/infdis/jiab461. PMC 9574657. PMID 34515290.
- ^ a b Kim WK, Cho S, Lee SH, No JS, Lee GY, Park K, Lee D, Jeong ST, Song JW (8 January 2021). "Genomic Epidemiology and Active Surveillance to Investigate Outbreaks of Hantaviruses". Front Cell Infect Microbiol. 10: 532388. doi:10.3389/fcimb.2020.532388. PMC 7819890. PMID 33489927.
- ^ a b c d e f g h i j k Jacob AT, Ziegler BM, Farha SM, Vivian LR, Zilinski CA, Armstrong AR, Burdette AJ, Beachboard DC, Stobart CC (9 November 2023). "Sin Nombre Virus and the Emergence of Other Hantaviruses: A Review of the Biology, Ecology, and Disease of a Zoonotic Pathogen". Biology (Basel). 12 (11): 1143. doi:10.3390/biology12111413. PMC 10669331. PMID 37998012.
- ^ a b c d e f g h Tariq M, Kim DM (March 2022). "Hemorrhagic Fever with Renal Syndrome: Literature Review, Epidemiology, Clinical Picture and Pathogenesis". Infect Chemother. 54 (1): 1–19. doi:10.3947/ic.2021.0148. PMC 8987181. PMID 35384417.
- ^ Klempa B, Avsic-Zupanc T, Clement J, Dzagurova TK, Henttonen H, Heyman P, Jakab F, Kruger DH, Maes P, Papa A, Tkachenko EA, Ulrich RG, Vapalahti O, Vaheri A. "Complex evolution and epidemiology of Dobrava-Belgrade hantavirus: definition of genotypes and their characteristics". Arch Virol. 158 (3): 521–529. doi:10.1007/s00705-012-1514-5. PMC 3586401. PMID 23090188.
- ^ a b c Riccò M, Peruzzi S, Ranzieri S, Magnavita N (25 October 2021). "Occupational Hantavirus Infections in Agricultural and Forestry Workers: A Systematic Review and Metanalysis". Viruses. 13 (11): 2150. doi:10.3390/v13112150. PMC 8621010. PMID 34834957.
- ^ a b c Afzal S, Ali L, Batool A, Afzal M, Kanwal N, Hassan M, Safdar M, Ahmad A, Yang J (12 October 2023). "Hantavirus: an overview and advancements in therapeutic approaches for infection". Front Microbiol. 14: 1233433. doi:10.3389/fmicb.2023.1233433. PMC 10601933. PMID 37901807.
- ^ a b c Hansen A, Cameron S, Liu Q, Sun Y, Weinstein P, Williams C, Han GS, Bi P (April 2015). "Transmission of haemorrhagic fever with renal syndrome in china and the role of climate factors: a review". Int J Infect Dis. 33: 212–218. doi:10.1016/j.ijid.2015.02.010. PMID 25704595.
- ^ Krüger DH, Schönrich G, Klempa B (June 2011). "Human pathogenic hantaviruses and prevention of infection". Hum Vaccin. 7 (6): 685–693. doi:10.4161/hv.7.6.15197. PMC 3219076. PMID 21508676.
- ^ Zhang Y, Ma R, Wang Y, Sun W, Yang Z, Han M, Han T, Wu XA, Liu R (30 September 2021). "Viruses Run: The Evasion Mechanisms of the Antiviral Innate Immunity by Hantavirus". Front Microbiol. 12: 759198. doi:10.3389/fmicb.2021.759198. PMC 8516094. PMID 34659193.
- ^ a b Sehgal A, Mehta S, Sahay K, Martynova E, Rizvanov A, Baranwal M, Chandy S, Khaiboullina S, Kabwe E, Davidyuk Y (18 February 2023). "Hemorrhagic Fever with Renal Syndrome in Asia: History, Pathogenesis, Diagnosis, Treatment, and Prevention". Viruses. 15 (2): 561. doi:10.3390/v15020561. PMC 9966805. PMID 36851775.
- ^ a b Lupuşoru G, Lupuşoru M, Ailincăi I, Bernea L, Berechet A, Spătaru R, Ismail G (September 2021). "Hanta hemorrhagic fever with renal syndrome: A pathology in whose diagnosis kidney biopsy plays a major role (Review)". Exp Ther Med. 22 (33): 984. doi:10.3892/etm.2021.10416. PMC 8311249. PMID 34345266.
- ^ Avšič-Županc T, Saksida A, Korva M (April 2019). "Hantavirus infections". Clin Microbiol Infect. 21S: e6 – e16. doi:10.1111/1469-0691.12291. PMID 24750436.
- ^ a b c d e f g h i j k l m n o p Koehler FC, Di Cristanziano V, Späth MR, Hoyer-Allo KJ, Wanken M, Müller RU, Burst V (29 January 2022). "The kidney in hantavirus infection-epidemiology, virology, pathophysiology, clinical presentation, diagnosis and management". Clin Kidney J. 15 (7): 1231–1252. doi:10.1093/ckj/sfac008. PMC 9217627. PMID 35756741.
- ^ Noack D, Goeijenbier M, Reusken CB, Koopmans MP, Rockx BH (4 August 2020). "Orthohantavirus Pathogenesis and Cell Tropism". Front Cell Infect Microbiol. 10: 399. doi:10.3389/fcimb.2020.00399. PMC 7438779. PMID 32903721.
- ^ a b c d e f g h i j Douglas KO, Payne K, Sabino-Santos G Jr, Agard J (23 December 2021). "Influence of Climatic Factors on Human Hantavirus Infections in Latin America and the Caribbean: A Systematic Review". Pathogens. 11 (1): 15. doi:10.3390/pathogens11010015. PMC 8778283. PMID 35055965.
- ^ a b c d e f g h i j k l m n o D'Souza MH, Patel TR (7 August 2020). "Biodefense Implications of New-World Hantaviruses". Front Bioeng Biotechnol. 8: 925. doi:10.3389/fbioe.2020.00925. PMC 7426369. PMID 32850756.
- ^ a b c d e Mustonen J, Henttonen H, Vaheri A (27 February 2024). "Hantavirus Infections among Military Forces". Mil Med. 189 (3–4): 551–555. doi:10.1093/milmed/usad261. PMC 10898924. PMID 37428512.
- ^ a b Tortosa F, Perre F, Tognetti C, Lossetti L, Carrasco G, Guaresti G, Iglesias A, Espasandin Y, Izcovich A (19 September 2024). "Seroprevalence of hantavirus infection in non-epidemic settings over four decades: a systematic review and meta-analysis". BMC Public Health. 24 (1): 2553. doi:10.1186/s12889-024-20014-w. PMC 11414058. PMID 39300359.
- ^ a b c d Meier K, Thorkelsson SR, Quemin ER, Rosenthal M (6 August 2021). "Hantavirus Replication Cycle-An Updated Structural Virology Perspective". Viruses. 13 (8): 1561. doi:10.3390/v13081561. PMC 8402763. PMID 34452426.
- ^ a b Tkachenko E, Balkina A, Trankvilevsky D, Kolyasnikova N, Teodorovich R, Vorovich M, Popova Y, Kurashova S, Egorova M, Belyakova A, Tkachenko P, Ishmukhametov A, Dzagurova T (13 August 2024). "The Specificity of Epizootic and Epidemiological Processes in Natural Foci of Hemorrhagic Fever with Renal Syndrome and Tick-Borne Encephalitis in Russia, as the Basis for the Prospects of Creating a Combined Vaccine for the Prevention of These Infections". Viruses. 16 (8): 1292. doi:10.3390/v16081292. PMC 11359185. PMID 39205266.
- ^ a b c d Moirano G, Botta A, Yang M, Mangeruga M, Murray K, Vineis P (July 2024). "Land-cover, land-use and human hantavirus infection risk: a systematic review". Pathog Glob Health. 118 (5): 361–375. doi:10.1080/20477724.2023.2272097. PMC 11338209. PMID 37876214.
- ^ Obando-Rico CJ, Valencia-Grajales YF, Bonilla-Aldana DK (January–February 2023). "Prevalence of orthohantavirus in rodents: A systematic review and meta-analysis". Travel Med Infect Dis. 51: 102504. doi:10.1016/j.tmaid.2022.102504. PMID 36402291.
- ^ a b c d e Tian H, Stenseth NC (21 February 2021). "The ecological dynamics of hantavirus diseases: From environmental variability to disease prevention largely based on data from China". PLoS Negl Trop Dis. 13 (2): e0006901. doi:10.1371/journal.pntd.0006901. PMC 6383869. PMID 30789905.
- ^ a b c "Genus: Orthohantavirus". ictv.global. International Committee on Taxonomy of Viruses. Retrieved 10 January 2025.
- ^ Bae JY, Kim JI, Park MS, Lee GE, Park H, Song KJ, Park MS (18 May 2021). "The Immune Correlates of Orthohantavirus Vaccine". Vaccines (Basel). 9 (5): 518. doi:10.3390/vaccines9050518. PMC 8157935. PMID 34069997.
- ^ a b Deng X, Tian S, Yu Z, Wang L, Liang R, Li Y, Xiang R, Jiang S, Ying T, Yu F (July–August 2020). "Development of small-molecule inhibitors against hantaviruses". Microbes Infect. 22 (6–7): 272–277. doi:10.1016/j.micinf.2020.05.011. PMID 32445882.
- ^ a b c Guardado-Calvo P, Rey FA (October 2021). "The surface glycoproteins of hantaviruses". Curr Opin Virol. 50: 87–94. doi:10.1016/j.coviro.2021.07.009. PMID 34418649.
- ^ a b LaPointe A, Gale M Jr, Kell AM (9 May 2023). "Orthohantavirus Replication in the Context of Innate Immunity". Viruses. 15 (5): 1130. doi:10.3390/v15051130. PMC 10220641. PMID 37243216.
- ^ a b c d e f g h Kuhn JH, Schmaljohn CS (28 February 2023). "A Brief History of Bunyaviral Family Hantaviridae". Diseases. 11 (1): 38. doi:10.3390/diseases11010038. PMC 10047430. PMID 36975587.
- ^ Kabwe E, Davidyuk Y, Shamsutdinov A, Garanina E, Martynova E, Kitaeva K, Malisheni M, Isaeva G, Savitskaya T, Urbanowicz RA, Morzunov S, Katongo C, Rizvanov A, Khaiboullina S (22 September 2020). "Orthohantaviruses, Emerging Zoonotic Pathogens". Pathogens. 9 (9): 775. doi:10.3390/pathogens9090775. PMC 7558059. PMID 32971887.
- ^ Klempa B (October 2018). "Reassortment events in the evolution of hantaviruses". Virus Genes. 54 (5): 638–646. doi:10.1007/s11262-018-1590-z. PMC 6153690. PMID 30047031.
- ^ "Virus Taxonomy: 2023 Release". ictv.global. International Committee on Taxonomy of Viruses. Retrieved 10 January 2025.
- ^ Kuhn JH, Bradfute SB, Calisher CH, Klempa B, Klingström J, Laenen L, Palacios G, Schmaljohn CS, Tischler N, Maes P (23 June 2023). "Reevaluate and reorganize family Hantaviridae (order Bunyavirales)" (docx). ictv.global. International Committee on Taxonomy of Viruses. Retrieved 10 January 2025.
- ^ "History of the taxon: Species: Orthohantavirus seewisense (2022 Release, MSL #38)". ictv.global. International Committee on Taxonomy of Viruses. Retrieved 10 January 2025.
- ^ Engdahl TB, Crowe Jr JE (15 July 2020). "Humoral Immunity to Hantavirus Infection". mSphere. 15 (4): e00482-20. doi:10.1128/mSphere.00482-20. PMC 7364217. PMID 32669473.


